Blood sugar, also called blood glucose, comes from eating or drinking carbohydrates and sugar. It supplies the muscles, brain and other organs with energy.
‘Your body aims to keep your blood sugar level in balance,’ says Dr Nikki Ramskill, a Livi GP. ‘With the central heating in your house, a thermostat is set so that when it’s too cold, the heating clicks on until it’s the right temperature again. Your body has a similar system, so when your blood sugar level is too low or high, hormones kick in to correct it.’
If you’re healthy, your sugar level looks after itself. Some people have a condition where you need to manage your blood sugar, known as diabetes.
How does diabetes affect blood sugar?
‘Diabetes is a serious condition where the body’s system for balancing blood sugar isn’t working properly,’ Dr Ramskill explains.
A hormone called insulin helps your body use blood sugar for energy. ‘Insulin allows the sugar in your bloodstream to enter your cells,’ says Dr Ramskill. ‘If you have diabetes, your body stops making or responding to insulin. The sugar gets stuck in the bloodstream, leading to higher blood sugar levels.’
Diabetes is common, affecting just under 1 in 10 adults.
What are the different types of diabetes?
The main types of diabetes are:
Type 1 diabetes: When you stop producing insulin and need to take regular injections to control your blood sugars.
Type 2 diabetes: When you still make insulin but stop responding to it. Blood sugars are managed by diet, activity or medication.
Prediabetes: When your blood sugars start to increase, which is a sign you are developing diabetes.
Gestational diabetes: When you have high blood sugar during pregnancy. This must be lowered to keep you and your baby healthy.
‘The advice varies for each type of diabetes, so it’s important to understand which one you have,’ says Dr Ramskill.
What is a normal blood sugar level?
For people without diabetes, blood sugar stays between 4.0 and 5.9 mmol/L.
‘Even in healthy people, blood sugar rises slightly after eating carbohydrates until hormones rebalance it. The swings are much greater for people with diabetes,’ explains Dr Ramskill.
What’s the target blood sugar for people with diabetes?
If you have diabetes, you should aim to keep your blood sugar within a certain range, usually:
- Before meals: 4.0 to 7.0 mmol/L
- 90 minutes after meals: 5.0 to 9.0 mmol/L
‘These ranges are generalisations,’ says Dr Ramskill. ‘A doctor will provide personal targets that are realistic for you.’
When you have diabetes, your blood sugar will sometimes go outside your target range. Here are some things that cause high or low blood sugar:
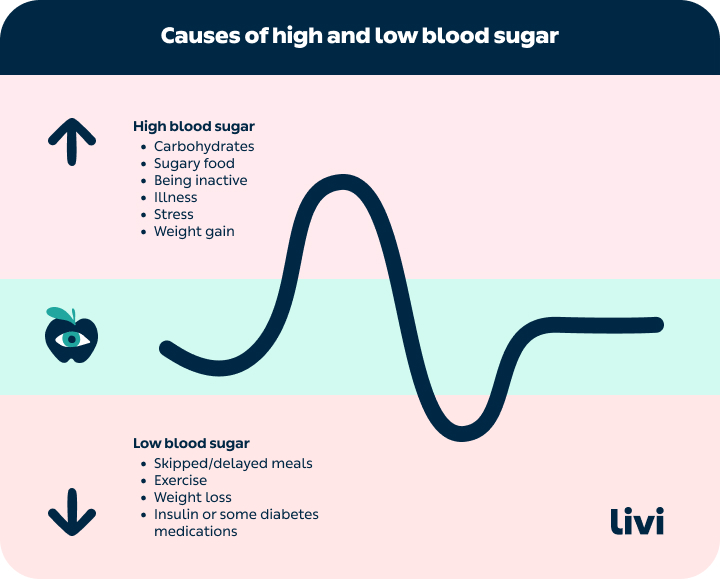
Some people need to check their blood sugar to make sure it doesn’t go too high or too low.
When should I check my blood sugar?
‘People usually only need to check their levels themselves if they take medication that causes low blood sugar, such as insulin or sulphonylureas,’ says Dr Ramskill. ‘How often you need to test depends on your diabetes type, lifestyle and which medication you take.’
It could be once a day or as many as seven times a day. A doctor can tell you how often to check and how to do it.
What happens when my blood sugar is too low?
Low blood sugar is less than 4.0 mmol/L, known as hypoglycaemia or a ‘hypo’. If you’ve got low blood sugar, you might have symptoms including:
- Hunger
- Shakiness
- Sweatiness
- Dizziness
- A racing heart
- Confusion, agitation or anxiety
Low blood sugar levels can be dangerous. It’s important to treat it quickly by eating or drinking a sugary snack and keeping an eye on your levels until they come back up.
What happens when my blood sugar is too high?
High blood sugar, also known as hyperglycaemia, can cause symptoms including:
- Feeling very thirsty
- Needing to pee a lot
- Blurry vision
- Frequent infections
If your sugar levels are high or you feel very unwell, you need to check for ketones or seek medical advice, as well as take action to lower your levels. Untreated high blood sugar can lead to a medical emergency.
Over time, even slightly high blood sugar can cause complications like kidney failure, nerve damage and strokes. Lowering your blood sugar to the target range helps reduce your risk of these things.
7 tips from a doctor for managing blood sugars
Managing your blood sugar levels helps keep diabetes from interrupting your life too much. Here are some recommendations on where to start:
1. Follow your care plan
‘Make sure you follow the advice from your care provider,’ says Dr Ramskill. ‘This may mean taking your medication properly, increasing activity or making healthier food choices.
‘It can be a big change, so you need to be honest with people in your life. Tell your friends, family and co-workers that you need certain allowances. They should support you to follow your care plan.’
2. Know your numbers
‘Depending on your type of diabetes, you may need to regularly measure your blood sugars, or you might need a regular check called a HbA1C test,’ says Dr Ramskill. Some people also look at their time spent in range, which shows the full highs and lows of their blood sugar.
‘Whichever way your blood sugars are monitored, it’s important to keep records. That way, you can see how your levels are changing and talk to your care provider about what’s working for you.’
3. Understand how different food affects your blood sugars
‘Some carbohydrates are simple – just a couple of sugars joined together to make a little molecule. They go into our bloodstream quickly and cause a large sugar spike,’ explains Dr Ramskill.
‘Other carbohydrates are more complex and take longer to break down, so when you eat them, your blood sugar doesn’t spike so high.’
To predict how different food affects your blood sugar, there are two main things to think about:
- How many carbohydrates am I eating?
- How long will this meal take to digest?
These two factors affect the glycaemic load of the meal, a measurement of how much it will raise your blood sugar. ‘Eating food with a high glycaemic load makes it harder to manage blood sugars,’ explains Dr Ramskill.
The table below gives you examples of glycaemic loads in different meals.
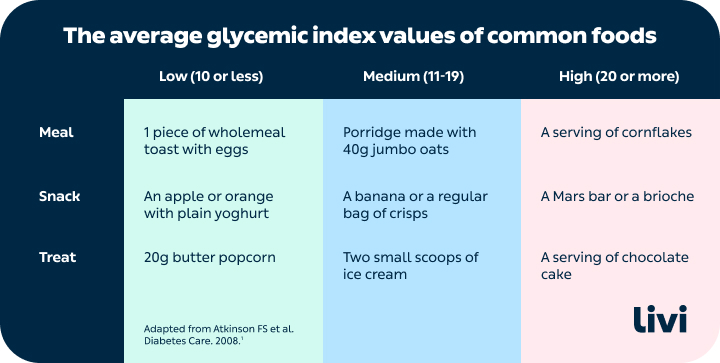
Adapted from Atkinson FS et al. Diabetes Care. 2008.
Eating foods high in fibre, fat or protein also slows down digestion to give a lower and slower spike. ‘Speaking to a dietician can help you to understand how different food affects you,’ says Dr Ramskill.
4. Learn how physical activity affects your blood sugars
In general, physical activity makes you more sensitive to insulin and so helps lower blood sugar. Even light activity, like walking, can make a difference. ‘For people with type 2 diabetes, an active lifestyle is an important part of their blood sugar management and can sometimes reverse their diabetes,’ says Dr Ramskill. ‘For type 1, it’s about being aware of how your insulin and exercise interact.’
Activity can raise or lower blood sugar depending on the duration and type of activity. If you take insulin or medication, speak to your care provider about how to avoid exercise-related hypos.
5. Make gradual changes
‘Make sustainable changes under the guidance of your care team. For type 2 diabetes, work towards a healthy lifestyle that you can keep up long term,’ says Dr Ramskill.
For type 1, keeping a blood sugar diary can help you to spot patterns so you can make gradual adjustments to your insulin.
6. Consider the bigger picture
Alcohol, stress, pregnancy, menopause, certain medications, fasting (like during Ramadan) and irregular sleep can all cause unpredictable effects on blood sugar.
‘A GP or diabetes team can help you tailor your approach to manage the more complicated side of blood sugars,’ says Dr Ramskill.
7. Be kind to yourself
Looking after your blood sugar can feel like a full-time job. ‘Diabetes burnout is a very real thing. Be kind to yourself and know that your control won’t always be perfect,’ reassures Dr Ramskill. ‘If you’re feeling overwhelmed or losing motivation, speak to a doctor. They can give you extra support to get you back on track.’
What questions should I ask a doctor about my blood sugar levels?
Your care provider can help you to manage your blood sugars. When you speak to them, you might find it helpful to ask the following questions:
- What are my target blood sugar ranges throughout the day?
- How often should I check my blood sugar levels?
- What do these numbers mean?
- What changes need to be made to my diabetes care plan?
If you think you may have undiagnosed diabetes or are struggling to manage your blood sugars, it’s important to speak to a doctor as soon as possible.
This article has been medically reviewed by Dr Nikki Ramskill, a Livi GP.


